Royal College of Psychiatrists call for more research into psychedelics for medical use
- Isabel Faulkner
- Sep 24, 2025
- 5 min read

By Isabel Faulkner
The Royal College of Psychiatrists (RCPsych) have released a position statement on the efficacy and safety of psychedelics and related substances (PARS), in addition to updated clinical guidance surrounding research into these compounds and a framework for delivering assisted psychotherapy. This report comes at a time when the resurgence of research into PARS is at its highest, with over 50 years of legal restrictions leaving a huge gap in pre-clinical knowledge. The RCPsych is a professional and educational body representing psychiatrists in the UK, who set the standards for the industry, and importantly advocate as a voice for psychiatrists, therefore making this report very impactful. Founder of Drug Science - Prof David Nutt welcomed the report: "We welcome the Royal College of Psychiatrists' landmark position statement, which marks a crucial step forward for the UK psychedelic medicine industry. Its call for a robust framework for delivering psychedelic-assisted psychotherapy aligns perfectly with our mission. We look forward to collaborating closely with the RCPsych to help develop these promising medicines for patients in need, building on this very positive foundation."
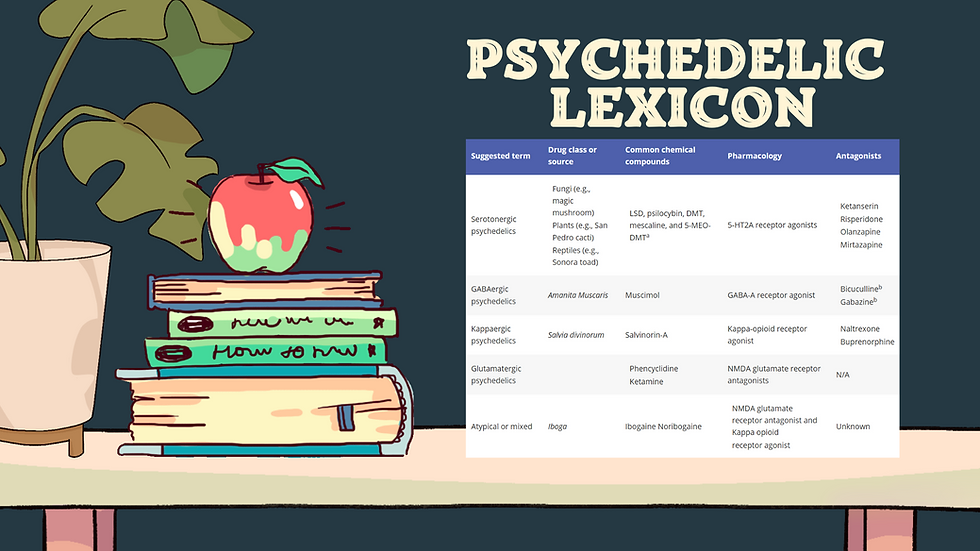
RCPsych acknowledge the heightened interest in PARS such as MDMA, LSD, ketamine, DMT, and psilocybin as treatments for mental health disorders, and additionally note the restrictions that have made research into these substances so difficult. The collated evidence is reviewed and the main message from the statement is that there is “currently limited high-quality evidence for the efficacy of these compounds”. Ketamine, however, and in particular the enantiomer [S]-Ketamine (esketamine) has had a large randomised controlled trial (RCT) conducted and so they recommend its use “in specialist settings with appropriate oversight and long-term monitoring arrangements in place” but still call for more research into any potential long-term side effects its potential efficacy for other psychiatric disorders.

On the contrary, at present, other countries are advancing in their policies surrounding PARS for certain conditions. Almost two years ago Australia legalised both psilocybin and MDMA for the treatment of certain mental health disorders, New Zealand expanded a compassionate access pathway to include psilocybin, and very recently Norway has approved funding for the use of intravenous (iv) ketamine for treatment resistant depression (TRD). The RCPsych agree that results look encouraging from clinical trials, including ketamine for TRD, MDMA for post-traumatic stress disorder (PTSD), ketamine for alcohol use disorder (AUD), and psilocybin for AUD. However, aside from ketamine they do not endorse routine clinical use of these compounds and warn of a “risk of claims jumping ahead of evidence”.
There was a continual call throughout the report for more pre-clinical evidence to elucidate the mechanism of action of these compounds, and additional clinical safety and efficacy trials. Given the emerging evidence for PARS use in patient psychotherapy sessions for a range of disorders, a greater understanding of the neurophysiological effects of these drugs is likely to be beneficial. It is critical to gain this pre-clinical evidence so that clinical trials can ensue, and patient benefit continue, however the ‘red tape’ surrounding the use of these drugs in research is limiting. The RCPsych do not call for the rescheduling of any of these compounds here. Author of the 'Red Tape' blog, and Chair of the Medical Psychedelics Working Group - Prof Joanna Neill has published multiple pieces of work on this issue and commented on this announcement saying: "I am delighted the RCPsych has released this very important position statement in support of Psychedelic Assisted Therapy for hard to treat conditions such as treatment resistant depression. However, while the RCPsych rightly identifies the need for more research on psychedelics, this report stops short of addressing the root cause: the UK's Schedule 1 classification and lack of research funding. This creates a scientific Catch-22 where we are told we need more evidence, but the government's restrictive scheduling and failure to dedicate funding for this research (in contrast to Australia, USA and Europe) actively prevents us from gathering it. Indeed it means that the much needed larger trials are being conducted in these countries where the law has changed, and the UK is being left behind. True progress requires the College to join us and others in advocating for rescheduling to unlock the essential research they themselves are calling for."
Another recommendation called for careful consideration of the “interplay between pharmacological effects… and the therapeutic relationship”. They emphasise the need for suitable set and setting of the psychotherapy and a multi-disciplinary team comprised of psychiatrists and therapists, along with a suitable curriculum prior to the session. The guidelines published highlight the need for a good therapeutic relationship between the patient and team and provide a framework for the most appropriate training and supervision. They recommend that a consultant psychiatrist, nurses, and psychologists form a team to review referrals for therapy, and at least two psychotherapists be present in the session.

They also propose that the RCPsych, along with other appropriate professional bodies, “take a leading role in developing specific training standards for the safe and effective delivery of this form of therapy”. We agree with this stance and propose that Drug Science is ideally positioned to partner with the RCPsych on its key recommendations. Our work on Project T21 with medical cannabis has given us unrivalled expertise in real-world data collection, making us the natural choice to help develop a national registry of psychedelic experiences. We would be delighted to combine our pharmacovigilance experience with the College's clinical expertise to co-create the professional standards and training necessary for safe and effective practice.
Key considerations:
It is clear from the RCPsych position statement that they wish to dampen the hype surrounding medical use of PARS. We agree that any medical use and advancement of clinical practice should always be substantiated by clear, scientific evidence, as is the ethos of Drug Science. However, the evidence for the use of these drugs in adjunct to therapy appears promising, and the research into this should not be held back. Indeed, the interplay between the action of the drugs and the psychotherapy is what may harness the ability of these compounds to be beneficial for certain conditions. We would never want to encourage recreational use of PARS without the therapy adjunct, which further highlights why more research is needed and why any decisions should be evidence led.
More research can only be facilitated if the restrictions are lifted. It is disappointing that the RCPsych did not call for rescheduling of these compounds because it would be the most effective way to remove research barriers and collate more evidence, which, they are calling for. It is perhaps unsurprising that ketamine is the furthest along in terms of having a large RCT and having robust evidence for its help in treating TRD, and it being the only drug amongst those listed that is schedule 2.
A multidisciplinary team is vital to delivering the most effective pharmacologically assisted psychotherapy. The RCPsych has laid out clear guidelines for psychotherapy assisted by PARS and highlights the importance of a highly trained specialist team. Additionally, they state that the professional training standards should be regulated by themselves and an appropriate professional body. This is something that we believe we have the most appropriate professional capacity for.